A dead tooth poses a serious health risk if left in the mouth. Having to constantly replace fillings can irritate, enlarge, and inflame the nerve within the tooth. As a result, over time, the living tissue in the center of the tooth can die. The empty space inside the tooth can become infected because cavities containing dead biological material are harmful to the body. This stuff decays over time, producing gases and liquids and causing further irritation. The tooth dies, and an abscess forms in the mouth as a result.
The problem is that these events take place in a very hard and non-expandable cavity inside the tooth. The fluids, gases, and bacteria within generate pressure, resulting in significant pain from the abscess. The abscess can erupt from the tip of the tooth into the bone, much like a volcano.
Infections that spread to the brain: How does it happen?
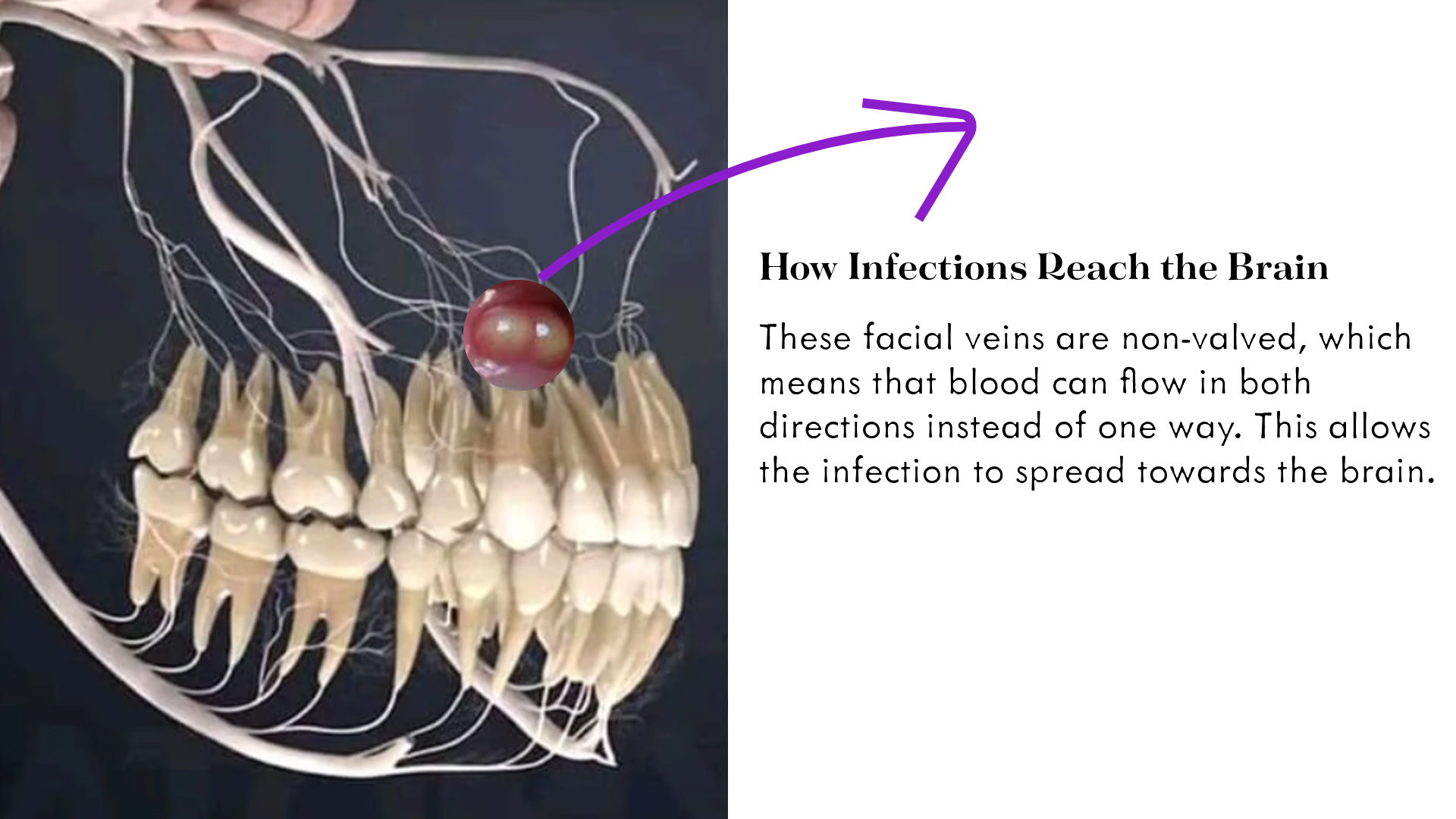
If an abscess remains untreated, the infection may disseminate to the bone surrounding the tooth, the jawbone, and subsequently to other regions of the body via blood vessels or sinus cavities. The tooth roots are closely connected to the vascular network in the face and head. Facial veins and arteries can carry infections to the brain, particularly from the teeth in the upper jaw. These facial veins are non-valved, which means that blood can flow in both directions instead of one way. This allows the infection to spread backwards, towards the brain.
Reported incidents
Former NFL player Mike Williams (36) died unexpectedly in September 2023. According to the Hillsborough County Coroner's Report, the cause of death was recorded as "bacterial sepsis due to multiple dental caries and tooth root debris with brain abscesses and necrotizing pneumonia." In other words, untreated dental caries and oral infections entered the bloodstream and caused a widespread infection (sepsis), resulting in the accumulation of pus in the brain tissue (brain abscess) and severe lung infection.
Tooth abscesses are a known cause of death for people like Mike Williams, but the exact number is unclear due to a lack of documentation. A young truck driver's heartbreaking story of his wife's death from a brain abscess was shown on ABC 10. Many neurosurgeons' anecdotes and accounts include comparable cases.
What are the symptoms of serious tooth infections?
Tooth infections may seem mild at first, but some symptoms may indicate that it could be serious. If you notice the following symptoms, you should consult a dentist:
- Pulsating pain: If you feel a constant, pulsating pain in the area of the affected tooth, this is a sign of infection.
- Red and swollen gums: Red and swollen gums indicate that the immune system is responding to the infection.
- Bad taste in the mouth: If you have a persistent bad taste, this may be related to the accumulation of pus in the infected area.
- Bad breath: Inflammation or decayed tissue can cause bad breath.
- Tooth discoloration: An infected tooth may turn gray or darker over time, indicating that the inner tissue of the tooth has been damaged.
- Hot-cold sensitivity: If you feel a sudden sharp pain when your tooth touches something hot or cold, this indicates irritation of the nerve tissue.
Serious Symptoms Requiring Immediate Intervention
The following conditions indicate that a dental infection has spread and urgent medical attention is needed. If you experience these symptoms, you should go to an emergency room:
- Fever: indicates that the body is fighting the infection and the inflammation is spreading.
- General weakness (malaise): Feeling weak and ill is a sign of a systemic infection.
- Swollen lymph nodes: Swollen lymph nodes, especially under the jaw or in the neck, indicate that the infection is spreading.
- Headache: May suggest that the infection may be affecting the sinuses or areas near the brain.
- Nausea or vomiting: Nausea may occur if the infection is affecting the body in general.
- Swelling of the face, neck or around the eyes: This indicates that the infection has spread severely and is life-threatening.
- Inability to open the mouth or jaw (trismus): A contraction of the jaw muscles may indicate that the infection has reached deeper tissues.
- Difficulty speaking, chewing or swallowing: Infection that has spread to the throat, tongue or jaw area can affect these functions.
- Difficulty breathing: If the infection affects the airways, this requires urgent medical attention.
- Rapid heartbeat: The heart rate may increase if the body is under stress due to high infection levels.
F.A.Q
Now let's deepen the topic with some topical questions and give it a little more depth.
How do you know when a dental infection has become fatal?
Dental infections, such as acute apical abscess, may initially be limited to the area around the tooth, but if left untreated can spread rapidly and lead to serious complications. The infection can spread to the fascial areas of the head and neck, leading to the development of cellulitis. Infection spreading along the jawbone and soft tissues can enter the bloodstream and spread throughout the body, leading to systemic infections.
Such spread can cause damage to organs and tissues as the immune system overreacts, a condition called sepsis. Sepsis occurs when microorganisms enter the bloodstream and if not treated in time, septic shock may develop, which may result in death with low blood pressure. Especially if there are symptoms such as fever, weakness, difficulty swallowing, shortness of breath, swelling of the neck or face, it is understood that the infection has spread beyond the local area and urgent intervention is required.
How long can you live with an infected tooth?
Numerous factors, including the kind of decay, its rate of spread, the tooth's size, and genetics, make it impossible to provide an exact duration for how long an infected tooth can stay in the mouth. Typically, this lasts between six months and two years. But in a matter of weeks, the inflammation can spread to the jawbone, adjacent tissues, and even distant organs if you don't treat it. Therefore, any sign of infection should be taken seriously and a dentist should be consulted immediately.
How fast can a dental infection spread to your brain?
Dental infections can spread rapidly and reach the head and neck region and even the brain. Infections from the upper jaw teeth, in particular, can travel in the opposite direction to the brain due to the non-valved vasculature. Although there is no clear timetable for how long it takes for the infection to spread to the brain, in some cases acute spread can occur within hours or days, which can have serious, even fatal consequences.
Can your body overcome a tooth infection on its own?
A tooth root infection will not go away on its own. Natural home remedies can only provide temporary relief. If the infection cannot be completely eliminated by the body, it can progress and worsen the condition. Professional treatment is essential for permanent recovery.
How long does a tooth hurt before the nerve dies?
The process of the tooth nerve dying can vary from person to person. During this process, throbbing and sharp pain may occur. As the tooth decay deepens, it reaches the nerve and vascular tissue and causes inflammation. The pain intensifies in the period before the nerve dies, and then may temporarily decrease for a while. However, the duration of this pain is different for each person.
How do I know if I have a brain infection from a tooth?
If a tooth infection has spread to the brain or other parts of the body, symptoms such as fever, fatigue, headache, nausea, confusion and excessive sleepiness may occur. Especially if there is difficulty swallowing, shortness of breath or severe swelling of the face and neck, it should be assumed that the infection has spread and medical attention should be sought immediately.
How quickly can sepsis develop from a tooth infection?
Sepsis due to tooth root infection can develop very quickly in some cases. Acute infections can quickly become systemic, causing the immune system to mount a full-body response. The initial symptoms of sepsis may be subtle, but can rapidly worsen. If left untreated, it can lead to septic shock and death. It is therefore vital to intervene without delay when signs of infection appear.
How long can a dead tooth stay in the mouth?
A tooth with dead pulp tissue can become infected over time. Although in some cases it can remain in the mouth for a long time without symptoms, this increases the risk of infection. The length of time a dead tooth can remain in the mouth without any symptoms depends on the individual situation, but it should always be evaluated by a dentist.
How long does it take for a tooth abscess to "burst"?
Dental abscesses develop over time as pus accumulates between the tissues. In some cases, the abscess may spontaneously open into the mouth and "burst". However, the process varies from person to person and can sometimes take weeks. Spontaneous drainage of the abscess usually provides temporary relief, but does not mean that the infection is completely cleared. Professional drainage and treatment are necessary.
How long can you live without noticing a brain abscess?
Brain abscesses can progress without symptoms. However, by the time symptoms such as headaches, changes in consciousness, and neurological problems appear, the condition may already be advanced. If not recognized early, it can be life-threatening. The risk of brain abscess in dental infections is low but possible. If there are suspicious symptoms, urgent evaluation is essential.
Conclusion;
It is almost impossible to talk about good body health without good oral health. The 2016 PAROKRANK study found that people with gum disease are 49% more likely to have a heart attack. Similarly, according to Harvard Health Press, people with gum disease are two to three times more likely to have a heart attack or stroke. Some academics assert that 50% of the 300,000 annual heart attacks in the United States are attributable to bacteria infiltrating the heart valves from dental plaque.
Whether it's cavities, abscesses, or dental plaque, maintaining good oral hygiene is key. These conditions can be effectively prevented—and often managed—by consistently following well-established, evidence-based dental care practices.
